Will having parathyroid surgery affect my thyroid? My thyroid function is normal, but I know someone who became hypothyroid after parathyroid surgery.

There are two issues that can occur with the thyroid: hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid). Both can occur after parathyroid surgery, but are both uncommon.
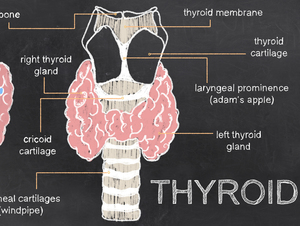
When we operate on the parathyroids, we are manipulating the thyroid somewhat - we may need to push it over to reach the parathyroids, for example. Most thyroids are fine with that, and most people will have no change in thyroid function after parathyroid surgery. Sometimes, the thyroid will be irritated with that, and you will get a postoperative thyroiditis. This is a temporary inflammation of the thyroid that produces hyperthyroidism (an overactive thyroid). This can create jitteriness, palpitations, and other symptoms of an overactive thyroid. (Note that low calcium can produce some of those symptoms also, so we will check calcium levels when checking thyroid hormone levels.) This usually lasts a few weeks, and then resolves on its own. For most people who have this, it is mild. Rarely, someone will have a cardiac arrhythmia like atrial fibrillation from hyperthyroidism, and need to be on a medication for that while it is resolving. This form of hyperthyroidism resolves on its own, usually in a few weeks.
Most people will not get postoperative hyperthyroidism, but it does occur. It is more likely in patients who already have “irritated” thyroid glands - such as Hashimoto’s thyroiditis or other chronic thyroiditis. These glands are less tolerant of any manipulation, and may be more likely to act up after parathyroid surgery.
The opposite problem, or hypothyroidism, is also uncommon. In most instances, the patients had borderline high TSH levels preoperatively, meaning that the thyroid was already somewhat hypothyroid, just not bad enough to start medication. For these patients, they likely would have started medication anyway, whether they had parathyroid surgery or not. The parathyroid operation may have just drawn attention to it. There is only one way in which parathyroid surgery could directly contribute to hypothyroidism: sometimes we need to clip one of the blood vessels that goes to the thyroid in order to control bleeding. This will reduce the blood flow to the thyroid. Normally this has a minimal long-term effect on the thyroid, because the thyroid has multiple blood vessels supplying it. But if the thyroid is already at the point where it is almost hypothyroid, this could contribute to becoming fully hypothyroid. I do not know of any other way in which parathyroid surgery could cause hypothyroidism, unless a large portion of the thyroid is removed at the same time.
Most patients who have no thyroid issues before parathyroid surgery will have no thyroid issues after parathyroid surgery. There are a small number of people who will get a temporary hyperthyroidism, and a smaller number who will develop hypothyroidism (but these were likely developing it already prior to surgery). Note that hypothyroidism overall is very common in adults. Patients with Hashimoto’s thyroiditis are at risk for temporary hyperthyroidism, but they are also at a high risk for long-term hypothyroidism, as the thyroid “burns out.” This is the natural history of the disease, whether you get parathyroid surgery or not.



